Thirty years ago, on June 5, 1981, AIDS was first acknowledged in print.
The article from the Centers for Disease Control wasn’t widely read, and it didn’t give a name to the disease. (It would be another year before scientists found one that fit, after giving several a try, including the terrible GRID, for “gay-related immune deficiency”.)
The paper certainly didn’t talk about HIV, since the virus wasn’t discovered until later. In fact, the article was mostly about the unusual appearance of Pneumocystis pneumonia in five young, gay men in Los Angeles. For all scientists knew, they were dealing with a superstrain of Pneumocystis that could eventually threaten the entire planet.
Well, they were half right.
At first, HIV and AIDS were a major setback for the burgeoning gay rights movement. Things had been moving swiftly for the community until then: the American Psychiatric Association removed homosexuality from its list of diseases in 1974 — just five years after Stonewall — and we were being treated more fairly in the media. We were even featured on popular TV shows like Dynasty and Soap, and although those representations weren’t perfect, they were far better than the psychopathic killers and suicidal maniacs we’d played before.
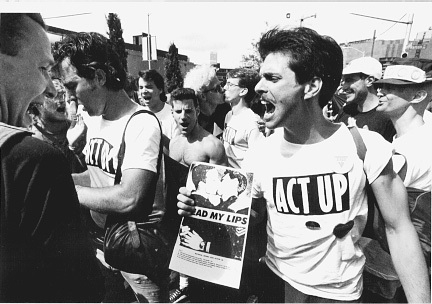
AIDS took the lives of many who campaigned for those achievements, and even people who weren’t ill were dumbstruck for a time. But grief is an unparalleled motivator, and soon, the LGBT community and its allies had formed sophisticated, efficient activist groups, pushing for treatment and prevention programs, destigmatization, and equal rights. We did as the ACT UP slogan said and turned our sadness into rage.
Over the course of the epidemic, roughly 30,000,000 people around the world have died from AIDS, and another 32,000,000 live with HIV/AIDS today. Treatment has gotten much easier and more bearable for those living with HIV, and there have especially promising developments in recent years, particularly in the area of stem cells and genetic therapy. But there is still no cure.
Take a moment today to think of your friends, family members, and neighbors who have died from AIDS or who are living with HIV/AIDS. Renew your commitment to wiping out this disease. Contribute to a local hospice, sign up for a charity walk, send a letter to your elected officials — whatever fits your style.
Everyone thought that AIDS would be cured by now. Let’s make certain that happens within the next 30 years — or hopefully, far sooner.
[Reposted from the lovely Sturtle. For those who have time, here is the original article from June 5, 1981 (or on the CDC website).]
Pneumocystis Pneumonia — Los Angeles
In the period October 1980-May 1981, 5 young men, all active homosexuals, were treated for biopsy-confirmed Pneumocystis carinii pneumonia at 3 different hospitals in Los Angeles, California. Two of the patients died. All 5 patients had laboratory-confirmed previous or current cytomegalovirus (CMV) infection and candidal mucosal infection. Case reports of these patients follow.
Patient 1: A previously healthy 33-year-old man developed P. carinii pneumonia and oral mucosal candidiasis in March 1981 after a 2-month history of fever associated with elevated liver enzymes, leukopenia, and CMV viruria. The serum complement-fixation CMV titer in October 1980 was 256; in may 1981 it was 32.* The patient’s condition deteriorated despite courses of treatment with trimethoprim-sulfamethoxazole (TMP/SMX), pentamidine, and acyclovir. He died May 3, and postmortem examination showed residual P. carinii and CMV pneumonia, but no evidence of neoplasia.
Patient 2: A previously healthy 30-year-old man developed p. carinii pneumonia in April 1981 after a 5-month history of fever each day and of elevated liver-function tests, CMV viruria, and documented seroconversion to CMV, i.e., an acute-phase titer of 16 and a convalescent-phase titer of 28* in anticomplement immunofluorescence tests. Other features of his illness included leukopenia and mucosal candidiasis. His pneumonia responded to a course of intravenous TMP/.SMX, but, as of the latest reports, he continues to have a fever each day.
Patient 3: A 30-year-old man was well until January 1981 when he developed esophageal and oral candidiasis that responded to Amphotericin B treatment. He was hospitalized in February 1981 for P. carinii pneumonia that responded to TMP/SMX. His esophageal candidiasis recurred after the pneumonia was diagnosed, and he was again given Amphotericin B. The CMV complement-fixation titer in March 1981 was 8. Material from an esophageal biopsy was positive for CMV.
Patient 4: A 29-year-old man developed P. carinii pneumonia in February 1981. He had had Hodgkins disease 3 years earlier, but had been successfully treated with radiation therapy alone. He did not improve after being given intravenous TMP/SMX and corticosteroids and died in March. Postmortem examination showed no evidence of Hodgkins disease, but P. carinii and CMV were found in lung tissue.
Patient 5: A previously healthy 36-year-old man with clinically diagnosed CMV infection in September 1980 was seen in April 1981 because of a 4-month history of fever, dyspnea, and cough. On admission he was found to have P. carinii pneumonia, oral candidiasis, and CMV retinitis. A complement-fixation CMV titer in April 1981 was 128. The patient has been treated with 2 short courses of TMP/SMX that have been limited because of a sulfa-induced neutropenia. He is being treated for candidiasis with topical nystatin.
The diagnosis of Pneumocystis pneumonia was confirmed for all 5 patients antemortem by closed or open lung biopsy. The patients did not know each other and had no known common contacts or knowledge of sexual partners who had had similar illnesses. Two of the 5 reported having frequent homosexual contacts with various partners. All 5 reported using inhalant drugs, and 1 reported parenteral drug abuse. Three patients had profoundly depressed in vitro proliferative responses to mitogens and antigens. Lymphocyte studies were not performed on the other 2 patients.
Reported by MS Gottlieb, MD, HM Schanker, MD, PT Fan, MD, A Saxon, MD, JD Weisman, DO, Div of Clinical Immunology-Allergy; Dept of Medicine, UCLA School of Medicine; I Pozalski, MD, Cedars-Mt. Siani Hospital, Los Angeles; Field services Div, Epidemiology Program Office, CDC.
Editorial Note: Pneumocystis pneumonia in the United States is almost exclusively limited to severely immunosuppressed patients (1). The occurrence of pneumocystosis in these 5 previously healthy individuals without a clinically apparent underlying immunodeficiency is unusual. The fact that these patients were all homosexuals suggests an association between some aspect of a homosexual lifestyle or disease acquired through sexual contact and Pneumocystis pneumonia in this population. All 5 patients described in this report had laboratory-confirmed CMV disease or virus shedding within 5 months of the diagnosis of Pneumocystis pneumonia. CMV infection has been shown to induce transient abnormalities of in vitro cellular-immune function in otherwise healthy human hosts (2,3). Although all 3 patients tested had abnormal cellular-immune function, no definitive conclusion regarding the role of CMV infection in these 5 cases can be reached because of the lack of published data on cellular-immune function in healthy homosexual males with and without CMV antibody. In 1 report, 7 (3.6%) of 194 patients with pneumocystosis also had CMV infection’ 40 (21%) of the same group had at least 1 other major concurrent infection (1). A high prevalence of CMV infections among homosexual males was recently reported: 179 (94%) had CMV viruria; rates for 101 controls of similar age who were reported to be exclusively heterosexual were 54% for seropositivity and zero fro viruria (4). In another study of 64 males, 4 (6.3%) had positive tests for CMV in semen, but none had CMV recovered from urine. Two of the 4 reported recent homosexual contacts. These findings suggest not only that virus shedding may be more readily detected in seminal fluid than urine, but also that seminal fluid may be an important vehicle of CMV transmission (5).
All the above observations suggest the possibility of a cellular-immune dysfunction related to a common exposure that predisposes individuals to opportunistic infections such as pneumocystosis and candidiasis. Although the role of CMV infection in the pathogenesis of pneumocystosis remains unknown, the possibility of P. carinii infection must be carefully considered in a differential diagnosis for previously healthy homosexual males with dyspnea and pneumonia.
References
- Walzer PD, Perl DP, Krogstad DJ, Rawson G, Schultz MG. Pneumocystis carinii pneumonia in the United States. Epidemiologic, diagnostic, and clinical features. Ann Intern Med 1974;80:83-93.
- Rinaldo CR, Jr, Black PH, Hirsh MS. Interaction of cytomegalovirus with leukocytes from patients with mononucleosis due to cytomegalovirus. J Infect Dis 1977;136:667-78.
- Rinaldo CR, Jr, Carney WP, Richter BS, Black PH, Hirsh MS. Mechanisms of immunosuppression in cytomegaloviral mononucleosis. J Infect Dis 1980;141:488-95.
- Drew WL, Mintz L, Miner RC, Sands M, Ketterer B. Prevalence of cytomegalovirus infection in homosexual men. J Infect Dis 1981;143:188-92.
- Lang DJ, Kummer JF. Cytomegalovirus in semen: observations in selected populations,. J Infect Dis 1975; 132:472-3.
